CASE REPORT | https://doi.org/10.5005/jp-journals-10030-1239 |
Primary Closure of a Complex Facial Wound with Underlying Fractures. Deconstructing Dogmas
Department of Trauma and Acute Care Surgery, Forbes Regional Hospital, Allegheny Health Network, Pennsylvania, USA
Corresponding Author: Saptarshi Biswas, Department of Trauma and Acute Care Surgery, Forbes Regional Hospital, Allegheny Health Network, Pennsylvania, USA, Phone: 412-858-2000, e-mail: saptarshibiswas@comcast.net
How to cite this article Biswas S. Primary Closure of a Complex Facial Wound with Underlying Fractures. Deconstructing Dogmas. Panam J Trauma Crit Care Emerg Surg 2019;8(1):64–69.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Canine bites present a major public health concern worldwide. Facial fractures due to dog bites are rare, although the exact incidence is unknown. Most reports in the literature comprises of pediatric population with a majority of the patients less than 5 years of age. Zygomatic, nasal, and orbital are the most frequently fractured bones. The dog breeds commonly responsible are American Pittbull and Rottweiler. The injuries can present as punctures, abrasions, tears, or avulsions. The intense kinematics of the crush injury can result in devitalized tissue, thus management becomes complex. Primary repair of these complex facial wounds can provide good cosmetic results. Controversy remains whether dog bites should be closed primarily and the indication for prophylactic antibiotics. Complex facial injuries cause functional and cosmetic impairment together with potential polymicrobial infections. They can also leave behind emotional scarring that can last long after the wound has healed. Antibiotics are indicated for infected bite wounds only and those of complex nature involving underlying bones, vascular structures, or joints. Tetanus immunization and potential risk of rabies should be considered in these patients.
Keywords: Dog bite, Maxillofacial fractures, Soft tissue injury.
RESUMEN
Las mordeduras de caninos representan un importante problema de salud pública en todo el mundo. Las fracturas faciales debidas a mordeduras de perro son raras, aunque se desconoce la incidencia exacta. La mayoría de los informes en la literatura comprende la población pediátrica con la mayoría de los pacientes menores de 5 años de edad. Cigomático, nasal, orbital son los huesos fracturados con mayor frecuencia. Las razas de perros comúnmente responsables son American Pittbull y Rottweiler. Las lesiones pueden presentarse como punciones, abrasiones, desgarros o avulsiones. La cinemática intensa de la lesión por aplastamiento puede resultar en tejido desvitalizado, por lo que el manejo se vuelve complejo. La reparación primaria de estas complejas heridas faciales puede proporcionar buenos resultados cosméticos. La controversia sigue siendo si las mordeduras de perros deben cerrarse principalmente y la indicación de antibióticos profilácticos. Las lesiones faciales complejas causan deterioro funcional y estético, junto con posibles infecciones polimicrobianas. También pueden dejar cicatrices emocionales que pueden durar mucho tiempo después de que la herida haya sanado. Los antibióticos están indicados solo para heridas por mordedura infectadas y aquellos de naturaleza compleja que involucran huesos subyacentes, estructuras vasculares o articulaciones. La inmunización contra el tétanos y el riesgo potencial de rabia deben considerarse en.
Keywords: Dog bite, Maxillofacial fractures, Soft tissue injury.
INTRODUCTION
Facial fractures associated with canine bites are rare, especially in adults.1 The exact incidence of facial dog bites with fractures is unknown. Heitz et al.2 in their case report published earlier this year mention of a total of 41 cases. Tu et al.1 mention that only 5% of the head and neck dog bites are associated with facial bone fractures. Zygomatic, nasal, and orbital are the most frequently fractured bones. Large breeds of canines can impart significant force 50–100 kg/cm2.3,4
Dog bites account for approximately 1% of all emergency room visits.5 Approximately 900,000 dog bites are treated in the United States each year.1 A majority of the victims are children. According to Foster and Hudson,6 45% of the attacks are caused by American Pit Bull Terriers. Rottweilers and German Shephards are also known to cause serious damage.8,9 According to the studies, 85% of the dog bites were from animals belonging to the victim and occur at or in the vicinity of the victims’ home as in our case.9–13
We report a case of an elderly woman who sustained significant facial lacerations with underlying nasal bone fractures which were repaired primarily. We discuss the dogmas of leaving dog bite wounds open, preemptive antibiotic use, and discuss the evidence-based management protocols.
CASE REPORT
A 85-year-old female was brought in as an activated level 2 trauma attacked by a “Great Dane” dog at her home. She reports that she was knocked into a wall and sustained several facial lacerations. She denies loss of consciousness (LOC). The dog is her daughter’s with updated vaccinations and is known to the patient.
Her past medical history composed of dementia, hypothyroidism, cervical radiculitis, primary osteoarthritis of the right shoulder, hiatal hernia, Barretts esophagus, hypertension, osteoporosis, macular degeneration with visual impairment, and right breast neoplasm. Her surgical history composed of breast lumpectomy with radiation, hysterectomy, laparoscopic femoral hernia repair, and tongue base reduction somnoplasty.
Her current medications were multivitamin with B complex and C, omeprazole, levothyroxine, and simvastatin. She was allergic to Neosporin, latex tape, and benzalkonium chloride. A former smoker she denied any alcohol or recreational drug use.
The patient was worked up in the usual Advanced Trauma Life Support (ATLS) protocol. Her airway was patent, breathing clear on auscultation. Her vitals were as follows: the blood pressure was 158/73 mmHg, the pulse rate was 93 beats per minute, the respiratory rate was 25 breaths per minute, and the SpO2 was 99%. She was oriented in time and place with a Glasgow Coma scale (GCS) 15. The secondary survey was essentially negative baring facial injuries. Although the conjunctivae and lids were normal, she had right periorbital ecchymosis, with several facial avulsions/lacerations over right eyebrow (Fig. 1), near the left eyelid medial canthus, across the nasal bridge and the cheek (Fig. 2). Visual acuity, pupillary evaluation, and visual field determination performed along with clinical evaluation of motility examination test eye movement in each of the six major gaze positions: left, right, up and in, up and out, down and out, and down were performed. No intraocular muscle entrapment signs were elicited. Hemotympanum was noted bilaterally, no midface instability, the nasal bridge was swollen but septum midline, dentition intact, and the trachea was midline. Compound fracture of the nasal bones was visible through lacerations with active bleeding from left angular vein and septal hematoma. Injection tetanus was administered in the trauma bay.
Rest of her review of systems were essentially normal.
Computerized tomography (CT) scan (Figs 3 and 4) showed bilateral displaced comminuted fracture involving the nasal bones along with extensive adjacent soft tissue swelling and subcutaneous emphysema. The ocular, intraorbital, and visualized intracranial structures are normal.

Fig. 1:: Facial laceration with deep puncture wound

Fig. 2:: Facial laceration with exposed nasal bone fragments
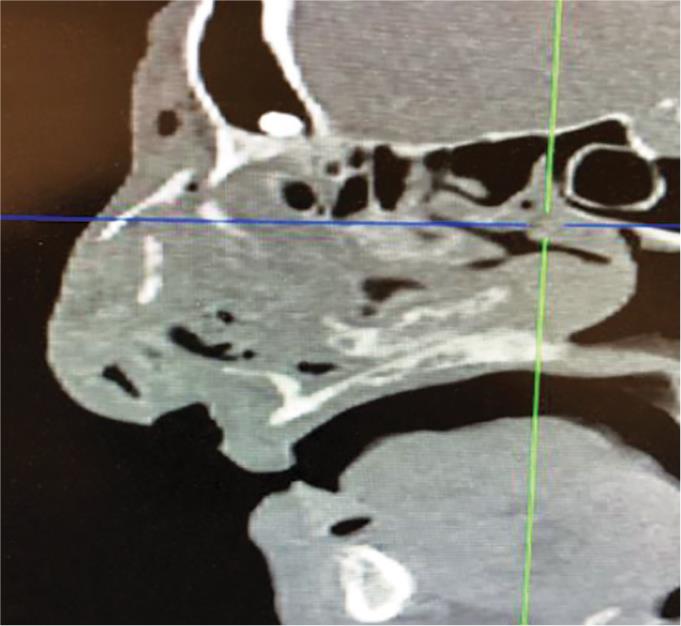
Fig. 3:: CT scan showing nasal bone fracture with subcutaneous emphysema

Fig. 4:: CT scan showing bilateral displaced comminuted fracture involving the nasal bones along with extensive adjacent soft tissue swelling and subcutaneous emphysema
THE OPERATION
Under general anesthesia, the patient was prepped and scrubbed with ophthalmic betadine. Her scrubbing was intensive with scrub brush searching for any area of necrosis and any area of devascularized tissue. Preoperative 2 g of IV ancef was administered. Intraoperative ENT consultation was sought.
The first laceration addressed was on the left side of the nose which has been bleeding actively. A large amount of blood was lost through a laceration at the end of a vein. The lateral aspect of the left side of the nose was explored. The vein was identified, clamped on either side and ligated .The wound, approximately 3 cm in size, was closed with a running 6-0 Vicryl for the subcutaneous layer followed by interrupted 6-0 Prolene for the skin.
The next laceration was 8 cm oriented almost horizontal, slightly oblique over the right eyebrow. There was plaque dissociation. These were then trimmed and debrided of all kind of necrotic tissue and hemorrhage in this area. A flap was then elevated into position and closed with a running 6-0 Prolene in a running fashion.
A vertical wound extending from the upper lip, medial to the medial canthus of the right eye was addressed. There was no obvious injury to the medial central tendon and an intraoperative probe was used to rule out nasolacrimal duct injury. Debridement of the nonviable tissue with ligation of bleeding vessels along with electrocoagulation was completed. The wound was closed with a running 6-0 Prolene.
The next major laceration addressed was an 8 cm wound extending from the dorsum of the nose along the lateral aspect of the nose and onto the cheek. Fractured nasal bones were definitely elevated out of position. Fragments of bone, which could possibly cause infection, were then carefully debrided and the fracture sites were held in position with monofilament sutures. The incision was then closed with 6-0 Prolene in a running fashion maintaining cosmetic approximation.
After these multiple lacerations were completed, left septal hematoma was cleaned and removed and there was a large laceration splitting the dome of the left side of the lower lateral cartilage. These were then approximated carefully in a horizontal mattress fashion, grasping skin, perichondrium, and finally perichondrium on the opposite side in skin. This was done to approximate the four different sutures. Postoperative images are shown in Figures 5 and 6.

Fig. 5:: Postoperative repair

Fig. 6:: Postoperative repair
The nose was not packed because of the situation with a dog injury. An external splint was used post closed reduction in the context of comminuted fracture, although the routine use is debatable. It was hard to determine whether these are claw marks or whether they are bite marks. Steri-Strips were put into all of these lesions and the patient extubated safely and was transferred to the recovery room for further postop care.
The patient was discharged the next day with a course of amoxicillin/clavulanate and reviewed in the clinic the following week and at 6 weeks. She was also followed up in the ENT clinic the next week post discharge and also at 6 weeks. Our patient was evaluated for nasal collapse and loss of tip support which were absent. She also underwent an outpatient ophthalmology checkup at 2 weeks. Her wounds were noted to be healed well.
DISCUSSION
Facial bites are complex injuries largely due to the functional and cosmetic importance of the location and often in addition to physical trauma which can result in potentially permanent disfiguring wounds it leaves behind a psychological and emotional trauma.14 Also besides, potential polymicrobial infections bites can also be a source of zoonotic infections particularly rabies and tetanus. The nose, cheek, and lips are commonly injured within the face.15
A dog bite can often be categorized into abrasions, puncture wounds, avulsions, crush injuries with underlying fractures, foreign bodies, and also nerve and tendon injuries.15 Modified Lackmann’s classification (Table 1) for facial wound can be used to assess the severity.16
The common dog bite causes a combination of tissue tears and adjacent punctures (“hole and tear” effect).17
Canine bites resulting in maxillofacial trauma should ideally be evaluated as an activated trauma according to ATLS guidelines.15,18,19 Imaging using CT scan is important in planning the optimal management.1,20 High index of suspicion for a fracture should be raised especially when large dog breeds are involved (Great Dane in our case) capable of crush injuries with considerable force.
Most infections associated with dog bites are polybacterial. Pasteurella is the commonest genus with Pasteurella canis being the predominant species.15,17 Gram positive bacteria are the commonest oral microorganisms found in canines and antibiotics should be tailored to cover Staphylococcus, Pasteurella, and Streptococcus.18 The anaerobes commonly found are Fusobacterium nucleatum, Bacteroides tectum, Prevotella heparinolytica, and Porphyromonas.17,21
According to current recommendations, amoxicillin/clavulanate is the prophylactic antibiotic of choice.15,18,22,23 For penicillin (PCN), allergy clindamycin plus either ciprofloxacin or trimethoprim– sulfamethoxazole (TMP-SMX) are used. The usual duration of therapy is 3–5 days and 10–14 days with bone involvement.15,16 Azithromycin is the most appropriate choice for penicillin allergic pregnant women. For heavily contaminated wounds with soil, intravenous therapy medications of choice are ampicillin-sulbactam or ticarcillin-clavulanate or cefoxitin. Intravenous (IV) antibiotics and hospitalizations may be indicated for immunodeficient patients, grossly infected wounds, or deep injuries with tendon exposure.
| Type | Clinical findings |
|---|---|
| I | Superficial injury without muscle involvement |
| IIA | Deep injury with muscle involvement |
| IIB | Full-thickness injury of the cheek or lip with oral mucosal involvement (through and through wound) |
| IIIA | Deep injury with tissue defect (complete avulsion) |
| IIIB | Deep avulsive injury exposing nasal or auricular cartilage |
| IVA | Deep injury with severed facial nerve and/or parotid duct |
| IVB | Deep injury with concomitant bone fracture) |
Administration of antibiotics can be prophylactic or therapeutic. Some authors have identified specific risk groups in whom prophylactic antibiotics may be indicated. These are presentation more than 8 hours after bite, bites involving face, genitalia, hand and feet, moderate to severe wounds, deep puncture wounds that may have penetrated joint spaces, bones or tendons, suspected fractures, and primarily closed wounds requiring surgical repair. The other group who would benefit includes diabetics, immunocompromised, elderly, asplenic, and patients with prosthetic heart valves.24
Small scattered bone fragments should be debrided because they can potentially form a nidus for infection. The oral cavity needs to be thoroughly inspected prior to general anesthesia especially in these facial traumas as fragments of teeth can be avulsed and swallowed causing potential damage of upper GI tract or airway obstruction.19
The time lag between the trauma and the commencement of treatment does have an impact while managing soft tissue injuries involving the head and the neck as delays can affect adversely the outcome.2 Earlier wound closure offers better results without increasing the wound infection rate. Many authors advise primary repair of uninfected wounds within the initial 24 hours of trauma for the best esthetic and functional results.7,24–26
Delicate, “tension-free” closure with thin synthetic materials should be practiced. In larger complex wound, deep sutures are minimized and often drains are used to obliterate dead spaces, thus reducing the possibility of infection. Stitches should be removed early around 5 days postoperative. We advocate irrigating the cavity with copious amount of saline with a 60 cc syringe to reduce contamination. Some authors prefer high-pressure pulse lavage especially during debridement of devitalized tissue to remove debris and fragments from the field and to reduce the bacterial load.8,27 Lacerated surfaces should be closed first approximating the wound edges to its correct anatomical orientation. In cases of significant tissue loss such as skin avulsions and amputations, reconstruction with plastic surgery expertise should be sought. Local patches, mucosal advances, divided skin grafts, or full thickness grafts can be performed.25 “Central target area” including the lips, nose, and cheeks often poses the greatest reconstruction challenges. The contours of the vermilion, commissure and the filter of the lips, the nasal margins, and nasal columella need complex reconstruction skills.28
Packing is an old method and is used less frequently now. Some of the reported complications attributed are postoperative pain, discomfort, soft palate laceration, septal perforation, and toxic shock syndrome.29,30 We decided following complete hematoma evacuation not to put in an anterior packing. Our plan was to reevaluate, in case the septal hematoma recurs. The closed nasal fracture technique, as was used in our case, depends on reversing the vector of force that resulted in the injury. A goldman bar is sometimes inserted into the nose up beneath the nasal bones and upward outward pressure applied. The combination of the intranasal pressure and the external digital manipulation helps maintain the force to reduce the nasal pyramid.31 Internal and external splints can be used postoperatively. Doyle splints, useful in internal splinting, help maintaining internal septal stabilization and prevent synechiae following surgery.32 Extranasal splinting helps maintain stabilization of reduced bones and cartilages usually after an open procedure.
Usually, the patients are followed up in the clinic in 6–12 weeks postoperatively as we did in our case. This time interval is often critical for the structural integrity of the nose.
Wu et al.33 looked at 86 pediatric patients with facial lacerations from dog bites. Wound were repaired in the ED (46%), the OR (51%), and outpatient settings (3%). All patients received antibiotics. No lacerations became infected. Paschos et al.34 found no infection in 41 wounds to the face (sutured or left open). Rich facial blood supply offers some protection against infection. The cosmetic benefit of facial closure likely outweighs the risk of infection, but each patient should be individualized.
Trauma in the periorbital region needs careful evaluation and often ophthalmology consultation.35 Orbital wall disruptions, enophthalmos, and entrapment of extraocular muscles causing diplopia may require surgical interventions.36
To check the status of tetanus, immunization is important. Patients not vaccinated within the last 5 years or incomplete %3C;3 immunizations or whose immunization records are lacking should get tetanus vaccination.37–40 Widespread vaccination of domesticated animals (as in our case) has reduced the incidence of rabies in household canines; it, however, remains a threat worldwide because of its high mortality. RPEP (postexposure prophylaxis) should be considered for all unprovoked animal bite victims as also for animals with unknown immunization status. These animals should be quarantined for 10–14 days during which prophylaxis should commence at the first clinical sign of the disease and/or any behavioral changes in the animal. Advisory Committee on Immunization Practices (ACIP) is the site to go for current recommendations regarding details of RPEP with human rabies immune globulin (RIG) and vaccines.41,42
We looked into evidence-based literature and tried to answer the frequently asked questions. Should we close dog bite wounds primarily or follow the traditional concept of leaving them open to heal by secondary intention? Is there truly an increased risk of infection associated with closing a dog bite injury?
Maimaris et al.43 in a prospective randomized trial in which 169 dog bites were managed by leaving the wound open vs closure with sutures. All wounds underwent thorough irrigation but either group received no antibiotics. Thirteen wounds (7.7%) became infected, six from the open group and seven from the sutured group. Wounds repaired %3E;10 hours postinjury and hand injuries (9/13) had an increased risk of infection. Chen et al.44 in a prospective observational cohort study of 145 mammalian bites (88 dog bites) that were closed primarily. Wounds were irrigated, 81% put on antibiotics. The subsequent wound infection rate of 5.5% was comparable to the clean laceration infection rate 3 to 7%. Rui-Feng et al.45 in a large randomized control trial (RCT) study (600 patients) randomized to closure vs no closure. Patients who presented with evidence of infection received antibiotics. All wounds were aggressively cleansed for at least 15 minutes. No statistically significant difference in wound infection was evident between closed and open wounds (6.3 and 8.3%, respectively). Paschos et al.34 presented with a RCT of dog bite wound management which composed of immunocompetent patients, who presented within 48 hours, and noncomplicated wounds without any underlying deep structure damage. One group (82 patients) had their wounds sutured, while the other (86 patients) had their wounds left open. All patients had their wounds pressure irrigated and received antibiotics (amoxicillin/clavulanate). There was no statistically significant difference in the rate of infection (8 vs 6 patients, respectively) but a significantly improved cosmetic outcome in patients whose wounds were sutured. Timing was also key with only 4.5% of patients developing an infection if presenting %3C;8 hours vs 22.5% of patients presenting %3E;8 hours developing an infection. These randomized controlled trials have shown no statistically significant increase in infection rates with closing dog bites vs leaving them open, than one would infer from such a stringent dogma. Hand infection rates are more compared to facial wounds.
CONCLUSION
Facial fractures resulting from dog bites are relatively uncommon. However, underlying fractures should be excluded in patients with bite injuries to the head or midface. This is more relevant when large breeds of dogs are involved capable of causing bite injuries with significant crush force. A computer tomography is the diagnostic modality of choice.
The treatment of these cases poses a significant difficulty not only from a technical purpose but also from an aesthetic and psychological angle and needs to handle with care. Multispeciality involvement may be warranted in complex cases. We advocate primary facial closure against the common notion of leaving the wound open. However, each case needs to be individualized and restorative treatment planned meticulously for the best outcome.
REFERENCES
1. Tu AH, Girotto JA, et al. Facial fractures from dog bite injuries. Plast Reconstr Surg 2002;109:1259–1265. DOI: 10.1097/00006534-200204010-00008.
2. Heitz C, Louzada GP, et al. Primary Repair of a Complex Panfacial Fracture by Dog Bite. Plast Reconstr Surg Glob Open 2018;6(4):e1719. DOI: 10.1097/gox.0000000000001719.
3. Wilberger JEJr, Pang D. Craniocerebral injuries from dog bite in an infant. Neurosurgery 1981;9:426–428. DOI: 10.1227/00006123-198110000-00015.
4. Lidner D, Marretta H, et al. Measurement of bit force in dogs to pilot study. J Vet Dent 1995;12:49–52.
5. Jerrard D. Bites (mammalian). BMJ Clin Evid 2006;05:914.
6. Foster MD, Hudson JW. Contemporary update on the treatment of dog bite: injuries to the oral and maxillofacial region. J Oral Maxillofac Surg 2015;73:935–942. DOI: 10.1016/j.joms.2014.12.003.
7. Wolff KD. Management of animal bite injuries of the face: experience with 94 patients. J Oral Maxillofac Surg 1998;56:838–843. DOI: 10.1016/s0278-2391(98)90009-x.
8. Morgan JP3rd, Haug RH, et al. Management of facial dog bite injuries. J Oral Maxillofac Surg 1995;53:435–441. DOI: 10.1016/0278-2391(95)90720-3.
9. Thompson PG. The public health impact of dog attacks in a major Australian city. Med J Aust 1997;167:129–132. DOI: 10.5694/j.1326-5377.1997.tb138810.x.
10. Ruskin JD, Laney TJ, et al. Treatment of mammalian bite wounds of the maxillofacial region. J Oral Maxillofac Surg 1993;51(2):174–176. DOI: 10.1016/s0278-2391(10)80017-5.
11. Goldstein EJ, Richwald GA. Human and animal bite wounds. Am Fam Physician 1987;36(1):101–109.
12. Griego RD, Rosen T, et al. Dog, cat, and human bites: a review. J Am Acad Dermatol 1995;33:1019–1029. DOI: 10.1016/0190-9622(95)90296-1.
13. Kizer KW. Epidemiologic and clinical aspects of animal bite injuries. JACEP 1979;8(4):134–141. DOI: 10.1016/s0361-1124(79)80339-1.
14. Peters V, Sottiaux M, et al. Posttraumatic stress disorder after dog bites in children. J Pediatr 2004;144:121–122. DOI: 10.1016/j.jpeds.2003.10.024.
15. Chhabra S, Chhabra N, et al. Maxillofacial Injuries Due to Animal Bites. J Maxillofac Oral Surg 2015 Jun;14(2):142–153. DOI: 10.1007/s12663-013-0593-5.
16. Kesting MR, Holzle F, et al. Animal bite injuries to the head: 132 cases. Br J Oral Maxillofac Surg 2006;44:235–239. DOI: 10.1016/j.bjoms.2005.06.015.
17. Talan DA, Citron DM, et al. Emergency Medicine Animal Bite Infection Study Group Bacteriologic analysis of infected dog and cat bites. N Engl J Med 1999;340(2):85–92. DOI: 10.1056/nejm199901143400202.
18. Stefanopoulos PK, Tarantzopoulou AD. Facial bite wounds: management update. Int J Oral Maxillofac Surg 2005;34:464–472. DOI: 10.1016/j.ijom.2005.04.001.
19. Goth S, Sawatari Y, et al. Management of pediatric mandible fractures. J Craniofac Surg 2012;23:47–56. DOI: 10.1097/scs.0b013e318240c8ab.
20. Wei LA, Chen HH, et al. Pediatric facial fractures from dog bites. Ophthal Plast Reconstr Surg 2013;29:179–182. DOI: 10.1097/iop.0b013e3182880114.
21. Goldstein EJC. New horizons in the bacteriology, antimicrobial susceptibility and therapy of animal bite wounds (editorial). J Med Microbiol 1998:47:95–97. DOI: 10.1099/00222615-47-2-95.
22. Goldstein EJ, Citron DM, et al. Comparative in vitro activity of faropenem and 11 other antimicrobial agents against 405 aerobic and anaerobic pathogens isolated from skin and soft tissue infections from animal and human bites. J Antimicrob Chemother 2002;50:411–420. DOI: 10.1093/jac/dkf139.
23. Abuabara A. A review of facial injuries due to dog bites. Med Oral Patol Oral Cir Bucal 2006;11:E348–E350.
24. Capellan O, Hollander JE. Management of lacerations in the emergency department. Emerg Med Clin N Am 2003;21:205–2310. DOI: 10.1016/s0733-8627(02)00087-1.
25. Javaid M, Feldberg L, et al. Primary repair of dog bites to the face: 40 cases. J Royal Soc Med 1998;91:414–416. DOI: 10.1177/014107689809100804.
26. Mcheik JN, Vergnes P, et al. Treatment of facial dog bite injuries in children: a retrospective study. J Pediatr Surg 2000;35:580–583. DOI: 10.1053/jpsu.2000.0350580.
27. Chisholm CD, Cordell WH, et al. Comparison of a new pressurized saline canister vs syringe irrigation for laceration cleansing in the emergency department. Ann Emerg Med 1992 Nov;21(11):1364–1367. DOI: 10.1016/s0196-0644(05)81903-1.
28. Palmer J, Rees M. Dog bites of the face: a 15 year review. Br J Plast Surg 1983;36:315–318. DOI: 10.1016/0007-1226(83)90051-6.
29. Fairbanks DN, Complications of nasal packing. Otolaryngol Head Neck Surg 1986;94:412–415. DOI: 10.1177/019459988609400337.
30. Stucker FJ, Ansel DG. A case against nasal packing. Laryngoscope 1978;88:1314–1313. DOI: 10.1288/00005537-197808000-00011.
31. Koca ÇF, Kizilay A. Management of nasal fractures. J Emerg Med Trauma Surg Care 2015,2:007
32. Doyle DE, House LF, et al. Description of a New Device: An Intra-nasal Airway/Splint. Laryngoscope 1997;87:608–612. DOI: 10.1288/00005537-197704000-00013.
33. Wu PS, Beres A, et al. Primary repair of facial dog bite injuries in children. Pediatr Emerg Care 2011 Sep;27(9):801–803. DOI: 10.1097/pec.0b013e31822c1112.
34. Paschos NK, Makris EA, et al. Primary closure vs non-closure of dog bite wounds. a randomised controlled trial. Injury 2014;45(1):237–240. DOI: 10.1016/j.injury.2013.07.010.
35. Coon D, Kosztowski M, et al. Principles for management of orbital fractures in the pediatric population: a cohort study of 150 patients. Plast Reconstr Surg 2016;137:1234–1240. DOI: 10.1097/prs.0000000000002006.
36. Oppenheimer AJ, Monson LA, et al. Pediatric orbital fractures. Craniomaxillofac Trauma Reconstr 2013;6:9–20. DOI: 10.1055/s-0032-1332213.
37. Lackmann GM, Draf W, et al. Surgical treatment of facial dog bite injuries in children. J Craniomaxillofac Surg 1992;20:81–86. DOI: 10.1016/s1010-5182(05)80472-x.
38. Graham WP3rd, Calabretta AM, et al. Dog bites. Am Fam Physician 1977;15:132–137. DOI: 10.1353/chapter.512253.
39. Goldstein EJC. Bite wounds and infection. Clin Infect Dis 1992:14:633–640. DOI: 10.1093/clinids/14.3.633.
40. Abuabara A. A review of facial injuries due to dog bites. Med Oral Patol Oral Cir Bucal 2006;11:E348–E350.
41. Rupprecht CE, Briggs D, et al. Use of a reduced (4-dose) vaccine schedule for postexposure prophylaxis to prevent human rabies. Recommendations of the Advisory Committee on Immunization Practices. Centers for Disease Control and Prevention. MMWR Recomm Rep 2010;59:1–19.
42. Centers for Disease Control Diphtheria, tetanus, and pertussis: recommendations for vaccine use and other preventive measures recommendations of the Immunization Practices Advisory Committee (ACIP) MMWR. 1991;40(RR-10):1–28.
43. Maimaris C, Quinton DN. Dog-bite lacerations: a controlled trial of primary wound closure. Arch Emerg Med 1988 Sep;5(3):156–161.
44. Chen E, Hornig S, et al. Primary Closure of Mammalian Bites. Acad EM 2000;7(2):157–162. DOI: 10.1111/j.1553-2712.2000.tb00519.x.
45. Rui-feng C, Li-song H, et al. Emergency treatment on facial laceration of dog bite wounds with immediate primary closure: a prospective randomized trial study. BMC Emerg Med 2013;13(Suppl 1):S2. DOI: 10.1186/1471-227x-13-s1-s2.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.